After a long delay, the U.S. Food and Drug Administration issued final regulations on August 16, 2022, for over-the-counter hearing aids. The final rule is effective 60 days from its publication, meaning that consumers could see OTC hearing aids hitting the shelves of community pharmacies nationwide by October 2022.
We are a pharmacist and audiologist who study the potential ways Americans with hearing loss can obtain OTC hearing aids. In a market dominated by only a handful of manufacturers, hearing aids that are now available without a prescription will expand access to the estimated 28.8 million U.S. adults who could benefit from their use.
A new class of hearing aids
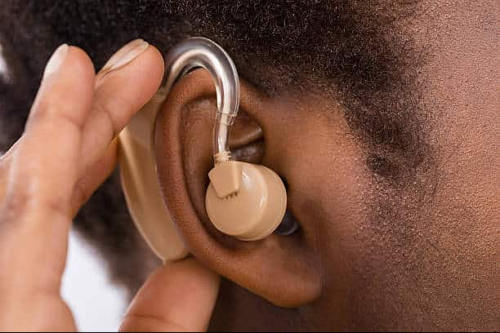
A hearing aid is a device worn around the ear that makes desired sounds more audible for people with hearing loss. Hearing aid devices include a microphone, amplifier, and miniature loudspeaker to make sounds louder. Traditionally, hearing aids have been accessible only with professional services provided by a licensed hearing aid dispenser or audiologist.
In 2017, the FDA Reauthorization Act designated a new class of hearing aids available over the counter to increase the accessibility and affordability of hearing aids for U.S. adults who believe they have mild to moderate hearing loss. These OTC hearing aids could be purchased without a medical evaluation by a physician or a fitting by an audiologist.
Before publishing the final rule, the FDA reviewed over 1,000 public opinions during the open comment period. The final ruling takes into account a variety of comments related to maximum sound output, product labeling, and user controls. Implementation of these regulations is a year overdue, largely because of the COVID-19 pandemic.
Audiologist practices are often located in urban centers that tend to have a smaller population of older adults.
Pharmacists will play a key role in OTC hearing aid sales. For one, pharmacies are more accessible to Americans than audiology practices. Audiologists tend to be located in metropolitan areas with higher incomes, younger populations, and greater insurance coverage, along with a smaller proportion of people who need hearing aids most – namely, older adults. In contrast, nearly 90% of Americans live within 5 miles of one of the more than 61,000 community pharmacies nationwide.
The ruling will also help get hearing aids into patients’ ears more quickly. It typically takes an average of four to five years after people recognize their hearing loss before they see a health care provider, and sometimes an additional six years to obtain a hearing aid device. With this new law, people will be able to purchase OTC hearing aids as soon as they become aware of their hearing difficulties.
OTC hearing aids will offer a do-it-yourself approach to addressing hearing loss. For example, people might be able to use a smartphone app to measure and adjust the hearing aid to best fit their hearing needs. Traditional hearing aids require a professionally administered hearing test and technical features that may allow more customized fine-tuning.
Increased access at lower costs
Hearing aid use among people who could benefit from their use remains low. The 2017 federal law may help remove barriers to hearing aid ownership by making them not only more accessible but also more affordable.
Prescription hearing aids cost, on average more than US $5,000 per pair, while the American Academy of Audiology predicts that OTC hearing aids will cost $300 to $600 per device. The charges and services associated with prescription hearing aids, which take an average of two to three audiology visits to acquire, are not typically covered by Medicare, Medicaid, or private insurers. At prices similar to monthly car loan payments, hearing health care services are often exclusive to people who have the means to pay high out-of-pocket expenses. Some hearing aids may be eligible for reimbursement using a flexible spending account.
Prohibitive costs and appointment hurdles can discourage patients from obtaining hearing aids.
There are also racial disparities in hearing aid use that could be mitigated by OTC hearing aids. Although Black Americans are more likely to have had a recent hearing test, they are less likely than white older adults to use hearing aids regularly. Such disparities can have potentially negative consequences for health and quality of life, including a higher risk of cognitive impairment, dementia, and falling, as well as social isolation, loneliness, and depression.
The pharmacist’s role in OTC hearing aids
While OTC hearing aids won’t require consultation with a medical professional or a hearing test, pharmacists will play an important role in ensuring their safe and effective use.
Community pharmacists, among the most accessible health care providers, are trained to identify, prevent and resolve medication problems. Pharmacists additionally have long helped patients purchase medical devices and equipment like glucometers for diabetes testing and blood pressure monitors for hypertension without a prescription.
Community pharmacists may soon be able to help patients pick out a hearing aid at their local pharmacy.
Community pharmacists are readying themselves to help patients select and purchase OTC hearing aids. In certain cases, pharmacists will refer some patients to audiologists and physicians for additional evaluation, treatment, and care. They may also follow up with patients to ensure the device works as expected. To prepare pharmacists for this new role, the University of Pittsburgh has developed an online program to teach pharmacists and pharmacy technicians how to help patients choose OTC hearing aids safely.
By providing a lower-cost and more readily available option, OTC hearing aids have the potential to address significant barriers to hearing aid adoption and use.
is a Professor of Audiology at the University of Pittsburgh Health Science. Lucas Berenbrok is an Associate Professor of Pharmacy and Therapeutics at the University of Pittsburgh Health Sciences. Both Mormer and Berenbrok write for The Conversation.